This was written a year ago. I never competely finished it, so I had never posted it. It has been a year, but today I am reflecting on that day one year ago.
Birth, like pregnancy and like parenthood, includes a lot of unknowns. When will my baby decide it’s time to enter the world? Is this real labor? Is this the best time? Nevertheless, it’s a process that I was ready for. There was certainly some fear. Was I prepared? Did I have my coping skills ready for labor? Will I be a good mom to this little boy? Will he make it so that I can hold him in my arms?
It took a lot to get to this point with him. Two miscarriages, grief, stress, obsession, lifestyle changes, millions of doctors, supplements, progesterone, biweekly blood draws. Was it possible that I could lose him after all that? I certainly hoped not, but I was aware of that possibility.
My birth plan was written, my doula was on stand-by, my midwife team was supportive. Work was at a place where it would be okay if I left, but it was definitely something that was on my mind a lot. By Wednesday – August 28th – I had all by two of my clients transferred. I had reports waiting to be signed but finished, and I had a few more things I could have liked to do. By Thursday morning, I still had notes to finish from Tuesday and Wednesday. I figured I could do them Thursday morning because I only had one transfer session scheduled that day. I was 38 weeks. I figured I would probably have a couple more weeks to work on more for the team – the average mom goes past her due date. I had made many documents preparing the team for my leave.
Rewinding a couple weeks, I had been having pretty intense and nearly constant back pain. Nothing seems to relieve the pain. I just had to cope with it. But it made me tired. It was very painful. I felt unprepared for childbirth. On August 19th, my back was hurting again as was typical, but I told Bryan that there was some pain that would intensify and go away. It didn’t feel like a big deal because it wasn’t terrible. Up until this point, I had taken the approach of “If I can ignore it, it’s not active labor.” Bryan asked if I was timing it. It really didn’t even dawn on me that I would want to do that, but I also didn’t think it was necessary. We headed out to OSF for infant CPR. I would glance at the clock when I felt the pain become a little more intense. Huh, they were about ten minutes apart. This didn’t feel like anything concerning though. Prodromal labor. I texted my doula with the irony of how this was happening while I was at OSF.
My doula is absolutely amazing and supportive. Her name is Kate. My experience would have been completely different if it wasn’t for her. She agreed that it sounded like prodromal labor. Prodromal labor is labor that starts and stops before active labor. The contractions are real, but they come and go and labor does not progress. I settled in working on comforts and coping skills and by the morning, the contractions were gone.
Prodromal labor continued most days over the next couple weeks. It would typically start as intense back pain that would stay constant, and by the evening, contractions would also start. The only thing that helped was falling asleep. Sleep was definitely more uncomfortable too. Sitting wasn’t comfortable and neither was laying. I would bounce on the ball or try different labor positions. In the end, I would continue this process for what felt like forever.
On Thursday, August 29, I woke up around 6:30am. I had just recently gotten up to go to the bathroom, but after lying back down, I felt something. I went to the bathroom again, and there was a lot of blood. I called for Bryan, and he shot awake. I also lost some kind of clump that was completely bloody. It almost seemed like a clot. I thought maybe it was my mucus plug or bloody show. But I thought I had already lost my mucus plug over a week again, and everything I had seen about blood show was streaked with blood, but this was an entire clump of blood. It was about 6:45 when I called Kate. She was at a client’s house for the night, and let me know she would call me back at 7 when she left. Bryan and I waited anxiously. Bryan was pretty nervous. He kept saying that Kate was taking too long. After talking to Kate, she recommended that I call my doctor’s office.
I called the after hours number shortly after 7. The nurse connected me to the midwife on call, Kristin. I remember being glad about that since she was one of the midwives that I liked. Kristin told me that she wanted me to be checked out, but that it could wait until the office opened. She instructed me to call the office when they opened in about an hour to schedule an appointment for an ultrasound and to meet with someone. I waited out the time by making breakfast and showering. I figured if we did need to go to the hospital, I would want to be well fed and ready. The office scheduled me for 9:00. I got my hospital bag ready and had Bryan put it in the car just in case.
The ultrasound went well. I was thankful that Ezekiel was okay. She said the fluid level looked good, the placenta looked good, and the baby was healthy. We waited until 9:30 to see Crystal, who I had never met with. She checked me and told me that I was 4 centimeters dilated. She checked again to be sure. This was the first time I had my cervix checked, so I didn’t know what it had been previously. Crystal wanted me to go to the hospital to be observed and be certain that my water had not broken since I still had some minor bleeding.
We called Kate to meet us at the hospital and headed over. Bryan dropped me off at the front before parking. I had some more food knowing that I probably wouldn’t be able to eat at the hospital. I remember thinking often how I really should have written those notes! We headed over to labor and delivery and got check into a triage room. Kate got there by the time I finished changing. The nurses were more concerned with asking a million questions to get my check updated. Kate explained that they still ask all these questions even if you come in having active labor, so it was helpful to get them out of the way now. I was having the intense back pain, but no contractions. After awhile, Mary Ann, a sweet triage nurse practitioner, came to check me and set up a plan. She said I was dilated to a 2. (Both said I was 90% effaced.) She got some samples to check if my water had broken. It didn’t. We waited forever to get another ultrasound to measure fluid levels, which were good. And we got to leave after about 4 hours.
I stayed home for the rest of the day, got my notes done, and sent out some emails just in case. I couldn’t decide if I should go to work the next day, and decided to wait to see how I was doing. I didn’t sleep much that night, but I fell asleep for at least an hour before I had another scheduled appointment on Friday morning. I was so tired, so I didn’t eat breakfast or shower so that I could sleep a little bit longer.
At the appointment, we met with Karen. She recommended a therapeutic rest. Kate had mentioned this as an option as well. Karen explained that the uterus may be so tired from the prodromal labor that allowing it to rest could either stop prodromal labor or kick start real labor. She prescribed me a medication with instructions to only take it if I had a minimum of five hours to sleep. I went to the chiropractor where she adjusted my pelvic bone as well explaining that it was shifted up. Based on Karen’s recommendation, I had some food, a lot to drink, took a bath, and then took the medicine. It was about noon when I took it.
I woke up about an hour later. I couldn’t go back to sleep. I laid in bed for about another hour before getting too uncomfortable and getting up. Contractions started to pick up and become more intense by 3:30. They felt more intense and were lasting about a minute but were still ten minutes apart. By 4:15 they were significantly more intense, were coming about every nine minutes, and required a lot more concentration.
By that point, I was no longer able to text Kate updates and Bryan took over at some point. The contractions got way more intense and I had to do a lot to move through them. By 5:00 or so, Bryan was trying to get the car packed and wasn’t sure if we should go to the hospital yet. During an intense contraction, I was able to get out that I felt like I was having trouble getting enough air. He finished packing up the car, and I made my way to the car.
I didn’t want to leave Bryan and he didn’t want to do valet parking, so I walked from where he parked with him to the front where we got a wheelchair. It was about 6:30pm at this point. As he wheeled me in, I asked if Kate was here yet.
“Uh.. I didn’t tell her to come yet.”
“Tell her to come now.”
I was definitely frustrated. This was real labor. This wasn’t like yesterday. We got up to labor and delivery and they rushed us into a random room because the triage rooms were full. I got changed into a gown, got into the bed, and immediately threw up red. Bryan and I were both a little freaked out. He called the nurse who calmly came in asking if I had anything red to eat.
Watermelon! Mystery solved. I wasn’t throwing up blood. Kate got there shortly after, but I don’t remember must about that point and didn’t realize she had gotten there. Bryan asked the nurse if I could have water. They said that wouldn’t help and would get an IV in. I remember the nurse checking me and saying I was 5 centimeters. I remember them asking me what I wanted for pain management.
Nothing.
I don’t really remember, but they tried desperately to get an IV in as I continued to throw up. Apparently I was super dehydrated at this point and the nurse blew every vein. I ended up with a huge bruise on that arm and she was never successful. As they wheeled my bed to a labor and delivery room, the nurse was shoving hot packs around my arm trying to get a vein to pop. I must have had my eyes closed, but I heard the nurse on the phone saying that she had a girl in active labor who didn’t want an epidural.
Things became more clear as I got into that room. The time was pretty blurred though. I focused on each contraction. I moved a ton in different ways that seemed helpful. I took direction from Kate and the nurse about different positions. The contractions were intense. Apparently they would frequently go off the chart. They were different than typical contractions. Rather than peaking once over the course of a minute, they would shoot you and stay high the entire time.
I remember Kate massaging my back a lot. My mom came too. Bryan was a great support but maybe overwhelmed by the process.
Karen was the midwife on call until the next day. She was pleased with how I was progressing.
Needed continual monitoring with one heart rate decrease from baby
Got to hospital 6:30ish 5cm
Water broke 9:30 at a 7
Heart rate dropped had to do continual monitoring at 11:30
12:30 – 8cm
12:45 talked about pitocin
2:45 agreed to epidural
Epidural 3:30
6:00am 9cm
12:30pm 10cm totally effaced
Pushing around 2:30
Born 5:26
Karen told me that we needed to have labor continue and it had been several hours where I had not progressed at all from 8cm. She waited as long as possible. She said she wanted to do this to give me an opportunity to still have a vaginal birth. She needed to start pitocin and wanted an epidural to give my body a chance to rest. She said my uterus was too tired to continue. They used a monitor in my uterus to measure contractions and get a better picture of how much potocin to use. They ended up needing to crank the pitocin up all the way and my contractions never got as high as they were before. But I did continue to progress. Pushing was productive. Ashley stayed nearly the entire time for pushing. It lasted three hours. I could feel when I pooped. After that I thought I could still feel poop stuck there but Kate explained that I was feeling the head. Pushing was very calm. After I got the hang of it, there was no counting or coaching. I pushed when I felt a contraction coming on. I closed by eyes and counted in my head for the count of three or four pushes. In between I completely relaxed and took a break. My eyes were closed for most of that too. At the beginning of pushing Ashley pointed out that my eye brows were wrinkled so I could completely relax. After that Bryan would rub my eye brow telling me how good I was doing.
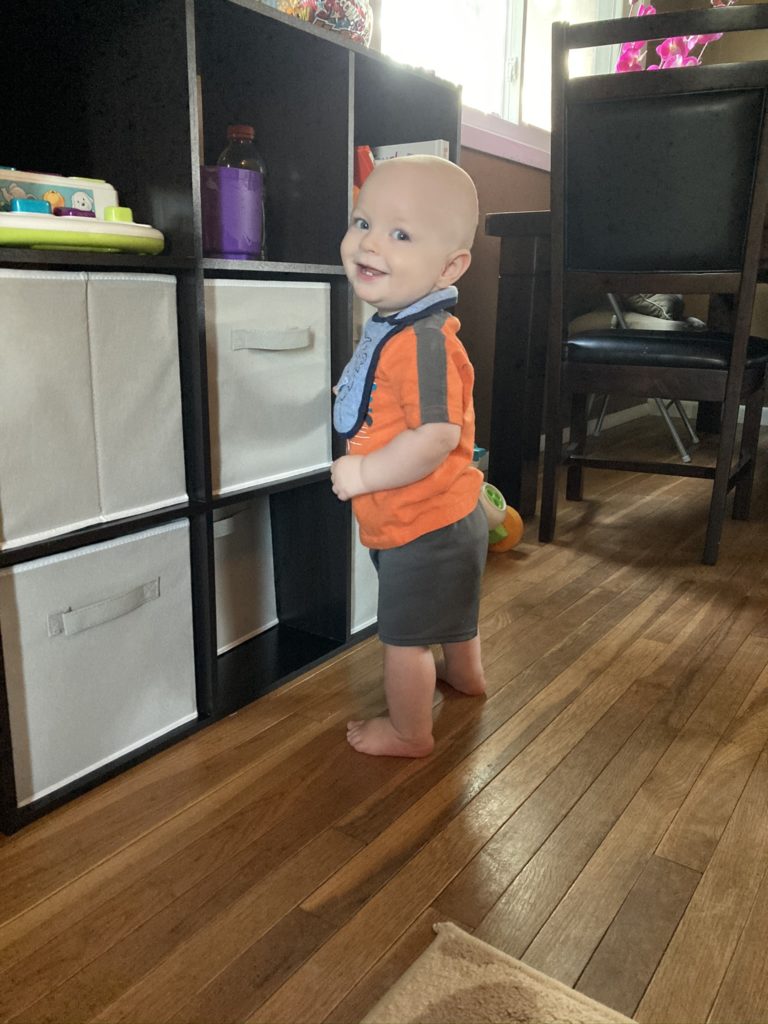
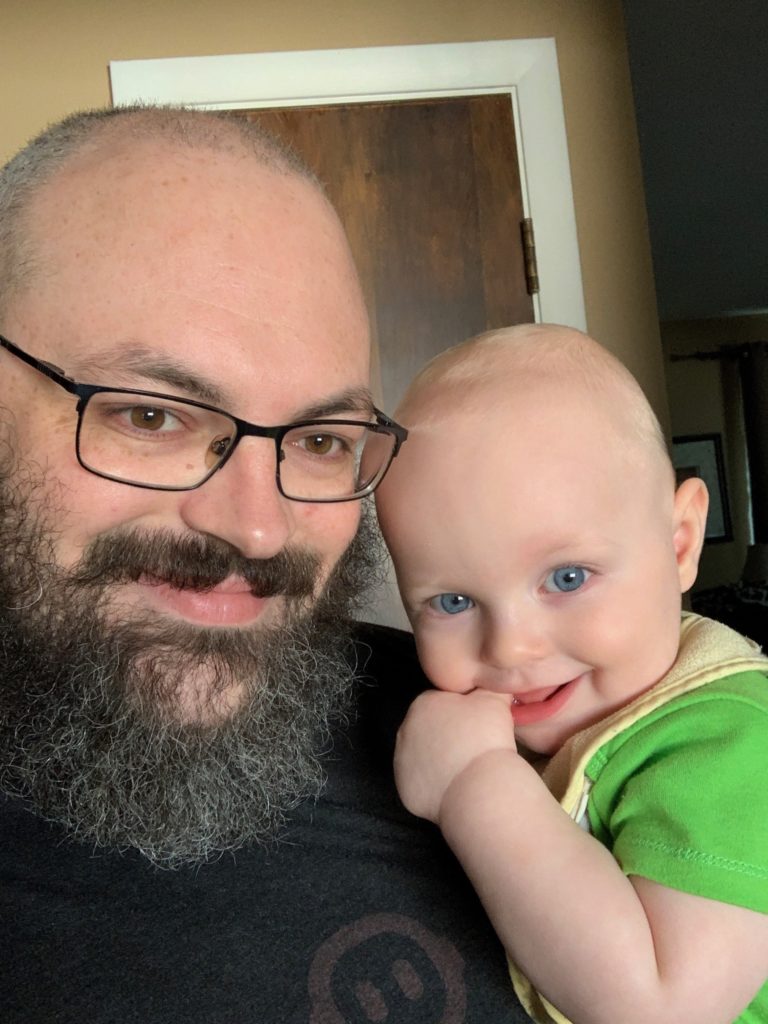
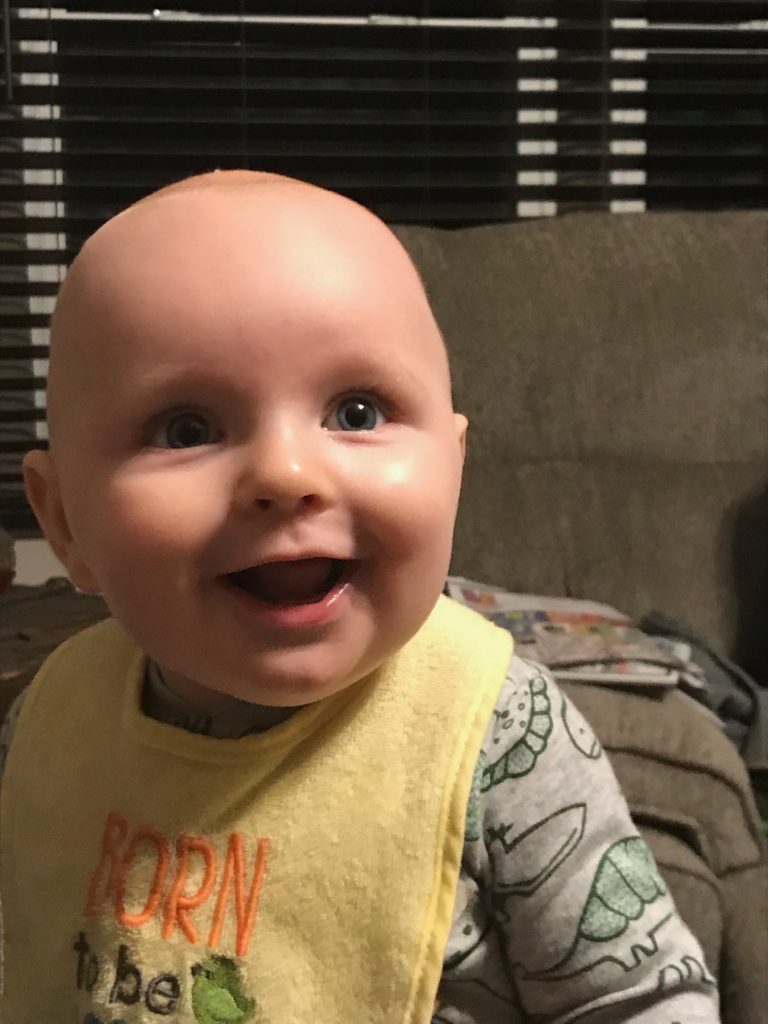
At the end, I felt the intensity of the need to push and just kept pushing without breaks. I opened by eyes enough to see a nurse coming around and shortly after Ezekiel was on my chest. Bryan described how crazy the process was. The two nurses came around and Kate stepped out of the way without saying anything. The nurses pushed my legs back. Another nurse pushed on my stomach hard. Then Ezekiel came out.
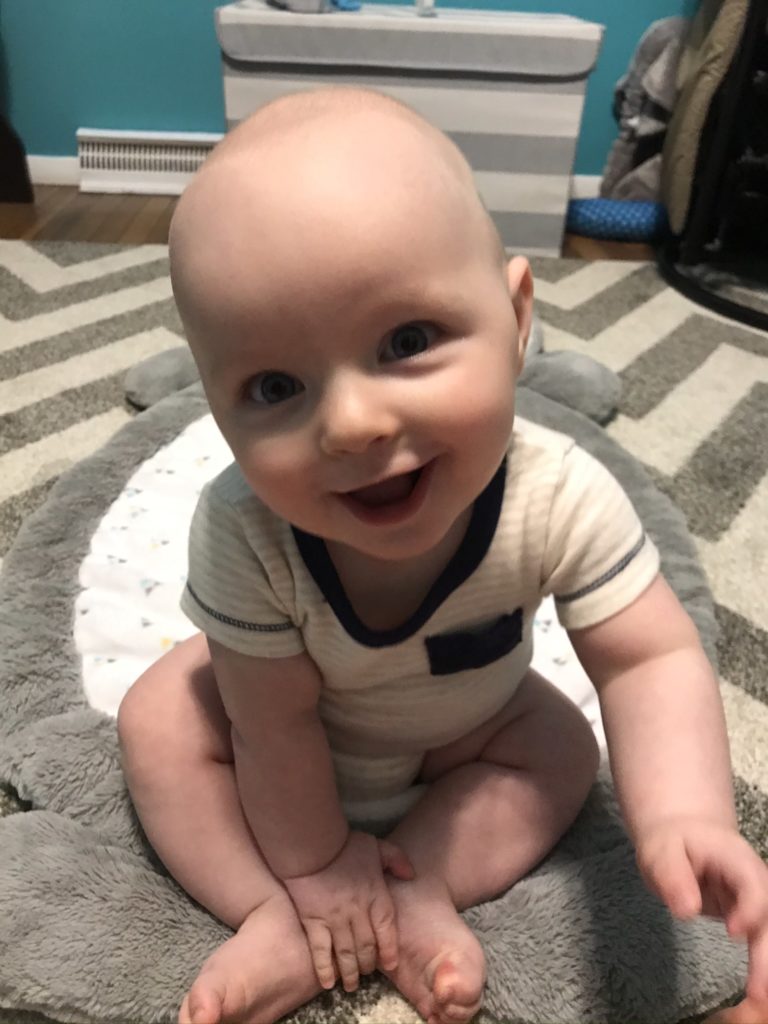
Turns out that Ezekiel’s shoulder was stuck. He had mild shoulder dystocia. They were able to get him out with only the first two interventions. We also found out why labor was so difficult. Ezekiel’s head was slightly off center. Therefore, his cone head was off centered too. He also had a subdural hematoma – blood had pooled in the back of his head from labor. He also had a true knot in his umbilical cord. Apparently these often cause fetal distress and seem to result in death frequently as well. Ezekiel was very lucky.
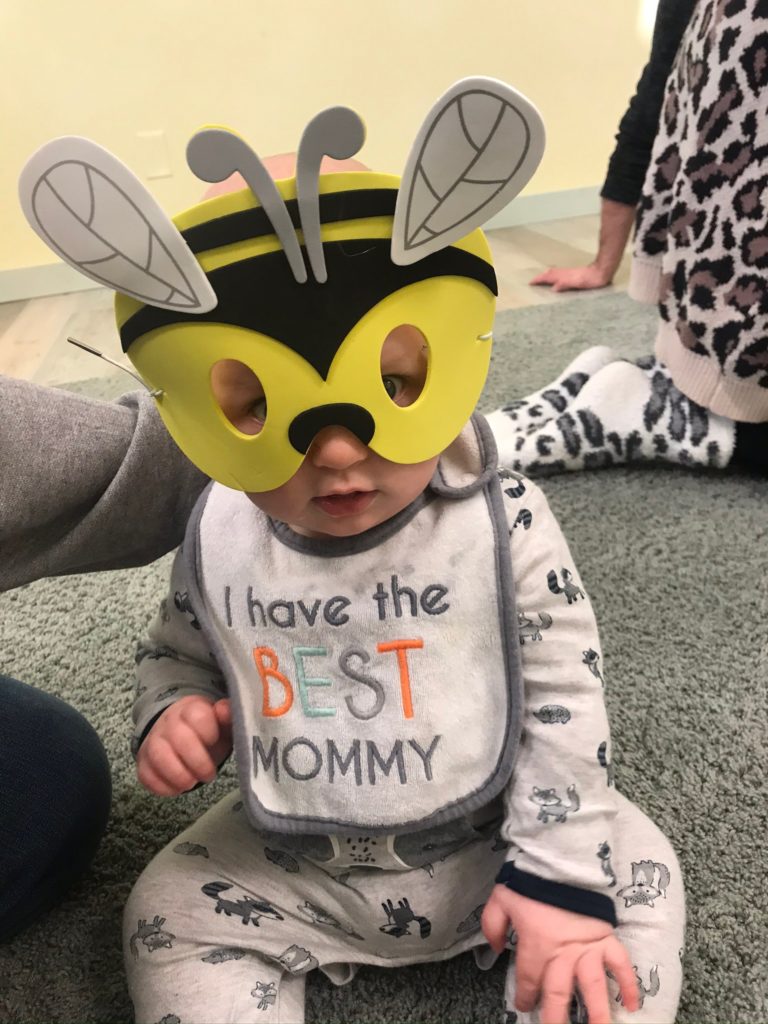
After holding him for a short while, the nurses were rubbing him down on my chest, and a doctor or nurse came up and told me that because of the shoulder dystocia, they needed to take him to the nursery and she asked if I was ready. I say no. I thought it was almost humorous looking back because of course I wasn’t ready, and I thought it was silly that she asked it that way. I also had no clue at that point that anything had gone wrong or that he even had shoulder dystocia. She agreed to do some of his shots on my chest but then said that she had to take him. Bryan went with him.
In the nursery they made sure that he did not have any broken bones and was breathing okay from the shoulder dystocia. He was good. They put marker on my head to measure the blood pooling and cone head making sure it went back. They measured several times throughout our stay.
When they brought him back to me, he was swaddled and could only stay a short time before going back to the nursery for more testing. He came back when I moved to the postpartum room.